Exercise, Insulin Pumps, and Hypoglycemia—A Practical Framework for Type 1 Diabetes
Why it matters
Exercise is one of the most common triggers for hypoglycemia in people with type 1 diabetes, particularly for those using insulin pumps and automated insulin delivery (AID) systems. Proactive, individualized insulin adjustments significantly reduce risk while preserving performance and confidence.
Key Recommendations (EASD / ISPAD / ADA)
Pre-Exercise
Target sensor glucose: 126–180 mg/dL (7.0–10.0 mmol/L)
Higher targets for those at increased hypoglycemia riskIf below target: 10–15 g rapid-acting carbohydrate
Mealtime bolus: Reduce by 25–75% depending on intensity, duration, and timing
Basal insulin: Reduce 10–50% or suspend pump for 1–2 hours
AID systems: Activate exercise mode 1–2 hours prior to activity
Clinical pearl: In select patients, a small manual bolus (~0.05 U) before exercise may reduce subsequent automated boluses
During Exercise
Use CGM/isCGM for real-time trend assessment
Keep rapid-acting carbohydrates readily available
Remember: AID systems help, but do not eliminate hypoglycemia risk
Post-Exercise
Reduce basal insulin by ~20% to mitigate delayed and nocturnal hypoglycemia
Correction boluses: Reduce by 50%
Avoid corrections near bedtime when possible
High-intensity or anaerobic exercise: Monitor for post-exercise hyperglycemia and correct conservatively
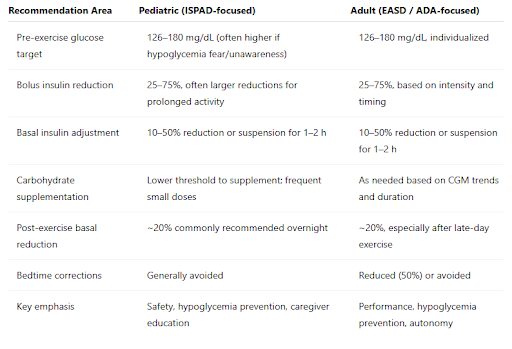
Table 1. Pediatric vs Adult Exercise-Related Pump Recommendations
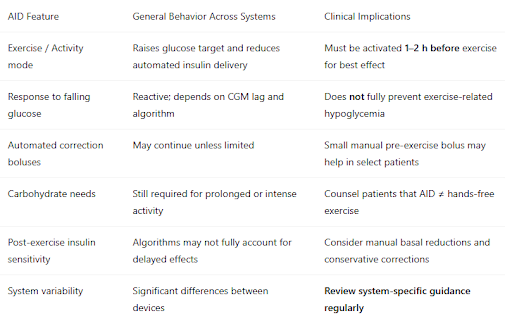
Table 2. Practical AID System Exercise Comparison (Consensus-Based)
Practical Clinical Pearl
Review—and keep a printed copy—of the EASD/ISPAD AID management “wheels” (linked here) outlining exercise recommendations for different AID systems in clinic.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11732933/
Having a quick-reference printout:
Improves real-time counseling
Reduces trial-and-error adjustments
Increases clinician confidence during busy visits
Think of it as the exercise playbook for insulin pumps.
Take-Home Message
Exercise is safest and most effective in type 1 diabetes when insulin pump strategies are anticipatory, individualized, and system-aware. CGM data, thoughtful insulin adjustments, and familiarity with AID behavior allow patients to move with confidence—on the field, in the gym, and in daily life.