When Glucose Isn’t the Villain: Rethinking Euglycemic DKA Management in the Age of Continuous Ketone Monitoring
When DKA Plays Hide-and-Seek
Classic diabetic ketoacidosis (DKA) tends to announce itself loudly—sky-high glucose, acidotic labs, and a clinical picture no one misses.
Euglycemic DKA (EDKA), on the other hand, whispers- with glucose levels that hover near normal, it’s a biochemical ninja: acidotic, ketotic, but not hyperglycemic enough to trigger alarm bells.
And yet, recent evidence suggests that our standard DKA playbook may not only be inadequate—it might be slowing recovery.
The emerging consensus?
EDKA demands more insulin, more dextrose, and more real-time insight—potentially via continuous ketone monitoring (CKM).
The Insulin–Dextrose Balancing Act: Flipping the Script
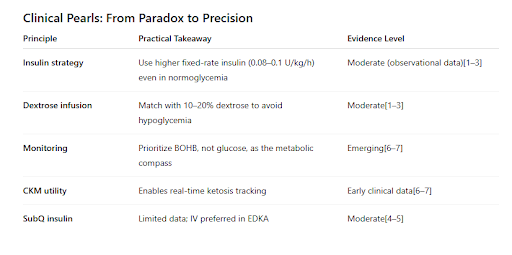
Traditional DKA protocols titrate insulin to glucose, reducing rates as glucose falls below 250 mg/dL. In EDKA, however, this strategy backfires. Glucose looks “fine,” but acidosis lingers because insulin doses are reduced too early.
Newer data and expert consensus suggest:
Use fixed-rate insulin infusions (0.08–0.1 units/kg/h).
Run higher dextrose concentrations (10–20%) to prevent hypoglycemia while maintaining that insulin drive needed to suppress ketogenesis.[1–3]
Lower insulin rates (≤0.05 units/kg/h) delay acidosis correction and prolong the anion gap.[2]
In short, think of it as “feed the insulin, not the glucose.”
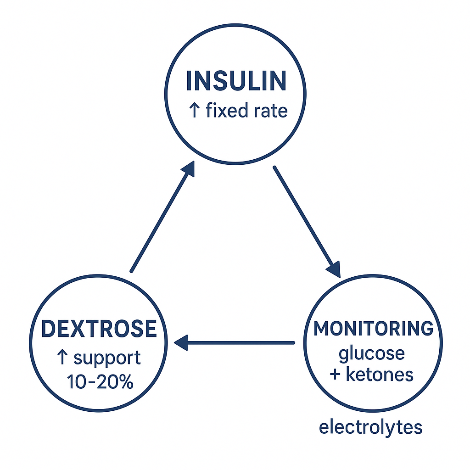
The EDKA Management Triangle
The arrows in the management triangle show balance among all three—raising dextrose enables higher insulin, which accelerates acidosis resolution, all under tight monitoring.
IV vs. SubQ: Know Your Battlefield
Subcutaneous rapid-acting insulin analogs are increasingly recognized as effective alternatives for mild to moderate classic DKA.[4–5]
But for EDKA? The data are thin. Given the atypical presentation and higher risk of delayed acidosis correction, intravenous insulin remains the standard of care, especially in hospitalized or critically ill patients.[4]
Still, for select stable patients in resource-limited or step-down settings, SubQ regimens may someday find a role—pending EDKA-specific trials.
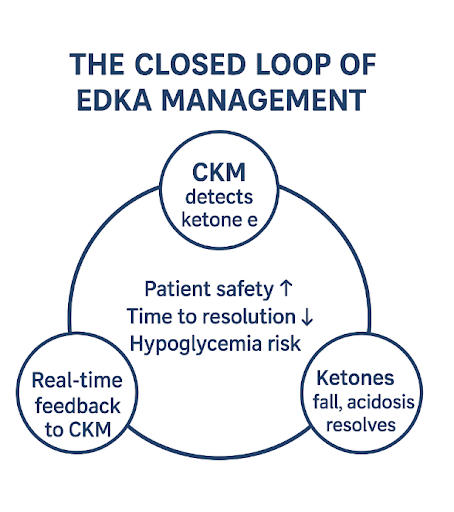
Continuous Ketone Monitoring: The Next Evolution
Continuous ketone monitoring could do for ketones what CGMs did for glucose; by measuring interstitial β-hydroxybutyrate (BOHB) every 5 minutes, they offer a dynamic window into ketosis trends.[6–7]
Potential advantages include:
Earlier detection of EDKA in patients on SGLT2 inhibitors or during pregnancy.
Real-time titration of insulin/dextrose infusions based on ketone clearance rather than just glucose.
Shorter time to resolution by avoiding under-treatment when glucose looks deceptively normal.
Clinical adoption is still nascent, and large outcome trials are pending, but the trajectory mirrors early CGM adoption: skepticism → evidence → standard of care.
The “New and Improved” closed loop of EDKA management
The Road Ahead: Ketones as the New Vital Sign
If glucose monitoring taught us anything, it’s that what you measure drives what you manage. For EDKA, glucose is only half the story. Ketones—particularly when tracked continuously—may become the true north of DKA management.
Until randomized data are available, the best approach may be pragmatic:
Go bold with insulin (safely).
Feed the insulin with dextrose.
Let ketones—not glucose—guide you home.
References
Cardona Z et al. Curr Diab Rep. 2025;25(1):48.
Albert SG et al. Diabetes & Metab Syndr. 2023;17(9):102848.
Barski L et al. Eur J Intern Med. 2019;63:9–14.
Diabetes Care in the Hospital: Standards of Care in Diabetes—2025. Diabetes Care. 2025;48(Suppl 1):S321–S334.
Lim BL et al. BMJ Open. 2023;13(2):e070131.
Kong YW et al. Diabetes Obes Metab. 2024;26 Suppl 7:47–58.
Jaromy M, Miller JD. Curr Diab Rep. 2022;22(10):501–510.